
Extremely high triglycerides can lead to a high risk of acute pancreatitis1,2
People with consistent fasting triglycerides >10 mmol/L (880 mg/dL) are in an established acute pancreatitis-risk danger zone1
Physical and emotional toll of acute pancreatitis
People with Familial Chylomicronaemia Syndrome (FCS) live in fear of painful, life-threatening acute pancreatitis attacks and emergency hospitalisations.3,4 One of the most common emotional symptoms of FCS is constant uncertainty about the possibility of acute pancreatitis or pain4
Even with treatment, extremely
high triglycerides take an emotional and social toll4
In a survey of 166 people with FCS, the most common emotional symptoms were:4

Uncertainty about acute pancreatitis or pain

Anxiety, fear, or worry about health

Uncertainty about what or how to eat

Feeling out of control because of their FCS
Extremely high triglycerides, such as those seen in FCS, can lead to acute pancreatitis risk2,3
Acute pancreatitis caused by extremely high triglycerides is often more severe and more fatal than acute pancreatitis caused by other factors5
Recurring episodes of acute pancreatitis are highly burdensome for people and healthcare systems:2,6,7
- Multiple episodes of acute pancreatitis can damage the pancreas, leading to chronic pancreatitis and diabetes2
Identifying those at risk of acute pancreatitis caused by high triglycerides is critical, because even one acute pancreatitis event dramatically increases the chance of a future one2
Just one meal can spike acute pancreatitis risk
Accumulation of chylomicrons (chylomicronaemia) from dietary fat can dramatically spike acute pancreatitis risk after just one meal8
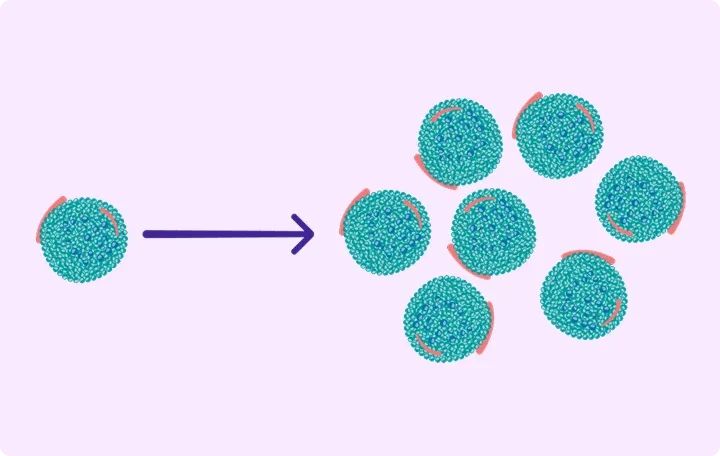
Triglycerides clearance can be saturated, and the body may be unable to clear additional dietary chylomicrons9
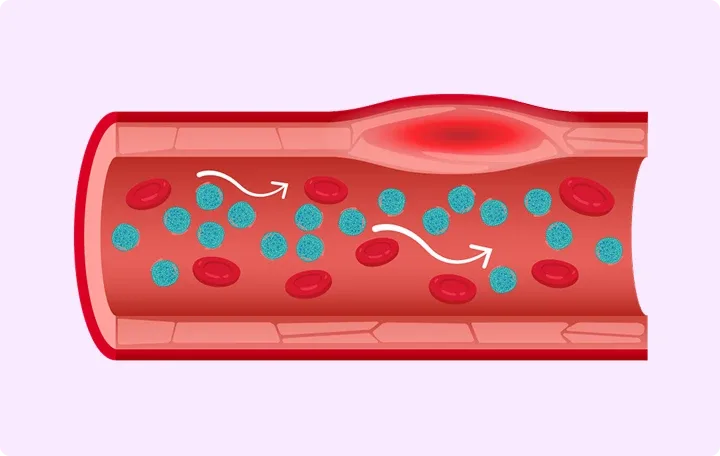
High levels of chylomicrons (chylomicronaemia) are thought to restrict blood flow and induce inflammation9,10
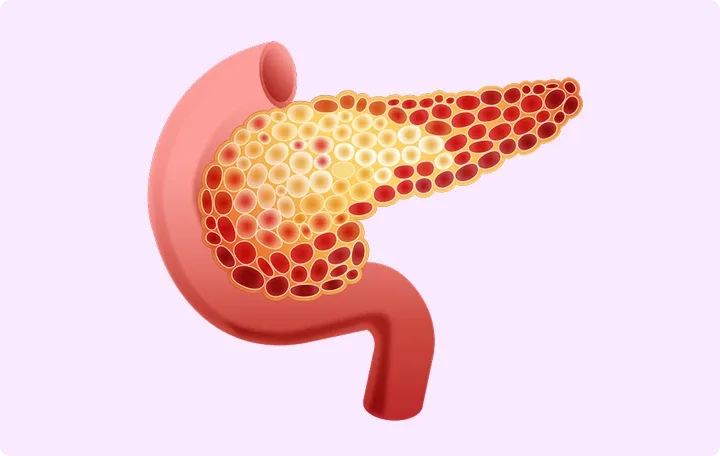
The pancreas may be particularly vulnerable to ischaemic damage caused by high levels of chylomicrons9,10
Scroll to Explore
Among people with triglycerides >11.3 mmol/L (1000 mg/dL), as seen in FCS, what proportion have experienced an acute pancreatitis event?*4,11
Thank you for your response.
Back*Data from hypertriglyceridaemia cohort studies11
Guidelines support the ≤10 mmol/L (880 mg/dL) target1
The primary goal of FCS treatment is lowering triglyceride levels to below the threshold for acute pancreatitis risk.1,6 The European Society of Cardiology and European Atherosclerosis Society guidelines establish that the risk of pancreatitis is clinically significant if triglycerides are >10 mmol/L (880 mg/dL)1
Approaches conventionally used to lower triglycerides, such as statins, fibrates, and omega-3 fatty acids have not been shown to lower the risk of acute pancreatitis in people with extremely high triglycerides6
The ESC/EAS Guidelines for the management of dyslipidaemias
RECOGNISE YOUR ROLE IN LOWERING THE RISK OF ACUTE PANCREATITIS
Early diagnosis and referral can make a difference for people with FCS
Discover more
Sign up for updates and more information
Receive the latest updates and insights about reducing triglycerides to ≤10 mmol/L (880 mg/dL)1
Abbreviations
AP, acute pancreatitis; EAS, European Atherosclerosis Society; ESC, European Society of Cardiology; FCS, Familial Chylomicronaemia Syndrome; TG, triglyceride.
Show References
- Mach F, Baigent C, et al. Eur Heart J. 2020;41(1):111–88.
- Sanchez RJ, Ge W, et al. Lipids Health Dis. 2021;20(1):72.
- Gaudet D, Stevenson M, et al. Lipids Health Dis. 2020;19(1):120.
- Davidson M, Stevenson M, et al. J Clin Lipidol. 2018;12(4):898–907.
- Garg R, Rustagi T, et al. Biomed Res Int. 2018;2018:4721357.
- Shamsudeen I, Hegele RA, et al. Expert Rev Clin Pharmacol. 2022;15(4):395–405.
- Guda NM, Trikudanathan G, et al. Lancet Gastroenterol Hepatol. 2018;3(10):720–8.
- Paragh G, Németh Á, et al. Lipids Health Dis. 2022;21:21.
- Goldberg RB, Chait A, et al. Front Endocrinol (Lausanne). 2020;11:593931.
- de Pretis N, Amodio A, et al. United European Gastroenterol J. 2018;6(10):649–55.
- Hernandez P, Passi N, et al. Curr Atheroscler Rep. 2021;23(11):65.