
Take aim at the true cause of their extremely high triglycerides1–5
Familial Chylomicronaemia Syndrome (FCS) causes extremely high triglycerides that are not lowered adequately by conventional triglyceride-lowering approaches (e.g., fibrates, statins, and omega-3 fatty acids)6–9
FCS CAUSES EXTREMELY HIGH TRIGLYCERIDES6-9
Extremely high triglycerides can be caused by genetic, metabolic, and lifestyle factors.8,10 Consistent fasting triglyceride levels >10 mmol/L (880 mg/dL) could be a sign of an underlying disease, such as FCS5,6
If extremely high triglycerides persist despite conventional approaches and lifestyle changes, consider FCS as the cause5,6
Not an actual patient
What is FCS?
FCS is a rare disorder with a global prevalence of 1 to 13 per 1,000,000. It may have a genetic cause, characterised by the absence of functional lipoprotein lipase in 80% of cases, but it is not always explained by known genetic causes11
Most conventional triglyceride-lowering approaches activate lipoprotein lipase, which is missing or non-functional in people with an underlying disorder such as FCS7–9,12
In unaffected individuals, lipoprotein lipase clears circulating triglycerides and chylomicrons from the blood shortly after a meal.4 In people with FCS, loss of lipoprotein lipase activity leads to the accumulation of triglycerides and chylomicrons (chylomicronaemia), resulting in fasting triglyceride levels at 10x-100x the normal level (fasting triglycerides >10 mmol/L [880 mg/dL] to >22.6 mmol/L [2000 mg/dL]) that only marginally lower with conventional triglyceride-lowering approaches2–4
Affecting ≥50% of people with FCS, acute pancreatitis is the most prevalent, severe, and potentially fatal complication13
Why conventional Triglyceride-lowering approaches are limited in FCS8,14,15
Tap to learn more
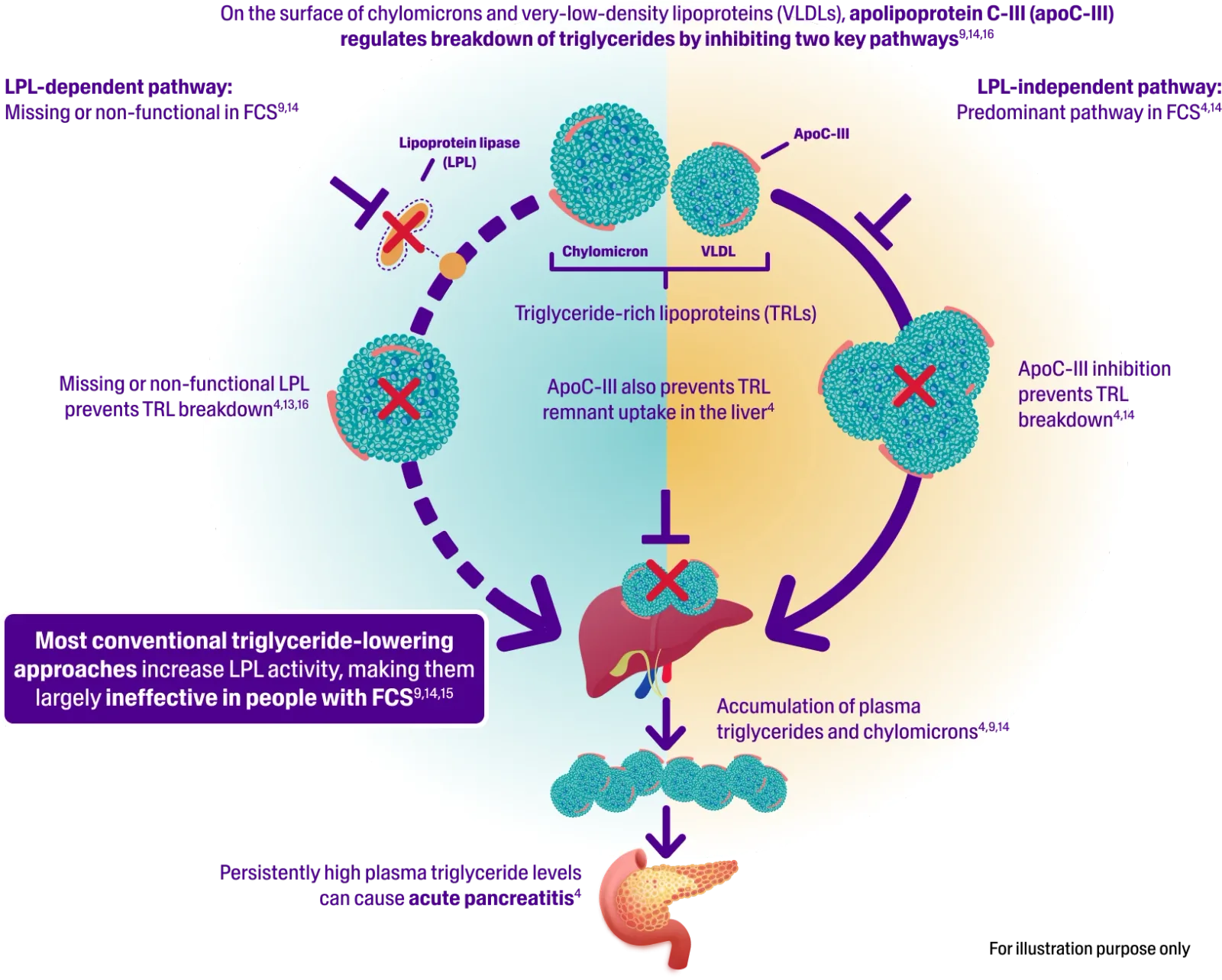
- Apolipoprotein C-III plays a key role in regulating triglyceride metabolism4,14
- It inhibits the breakdown of chylomicrons and clearance of subsequent triglycerides via both lipoprotein lipase-dependent and -independent pathways4
- Triglycerides are transported in the blood by chylomicrons and VLDL in the circulation4,15
- FCS is characterised by the absence of functional lipoprotein lipase in 80% of cases9
- The impaired clearance of chylomicrons from the bloodstream leads to chylomicronaemia and increased risk of acute pancreatitis4,13
Suspect FCS in people with extremely high triglycerides
Many cases of FCS are misdiagnosed because the nature of extremely high triglycerides is misunderstood. People with FCS tend to appear ‘normal’ – often experiencing acute pancreatitis attacks with no clear triggers9,17
In addition to causing acute pancreatitis, FCS can impact the liver, spleen, heart, and eyes, and cause other systemic problems9
Symptoms and comorbidities reported in a survey of 166 people with FCS:9
Tap a body part to learn more

- Difficulty concentrating (16%)
- Impaired judgment (11%)
- Lipemia retinalis (9%)
- Brain fog (8%)
- Forgetfulness (8%)
- Abdominal pain (41%)
- Acute pancreatitis (40%)
- Bloating (37%)
- Indigestion (27%)
- Diabetes (16%)
- Chronic pancreatitis (11%)
- Enlarged liver (hepatomegaly, 11%)
- Enlarged spleen (splenomegaly, 10%)
- Hypertension (10%)
- Feeling of physical weakness (asthenia, 30%)
- Eating disorders (23%)
- Fatigue (23%)
- Peripheral neuropathy (7%)
IN PEOPLE WITH EXTREMELY HIGH TRIGLYCERIDES WHO HAVEN’T RESPONDED TO CONVENTIONAL APPROACHES, THINK FCS6–9
Recognise the risk of acute pancreatitis
See the risk
Sign up for updates and more information
Receive the latest updates and insights about reducing triglycerides to ≤10 mmol/L (880 mg/dL)1
Abbreviations
AP, acute pancreatitis; apoC-III, apolipoprotein C-III; FCS, Familial Chylomicronaemia Syndrome; LPL, lipoprotein lipase; TG, triglyceride; TRL, triglyceride-rich lipoprotein; VLDL, very low‑density lipoprotein.
Show References
- Mach F, Baigent C, et al. Eur Heart J. 2020;41(1):111–88.
- Larsson M, Vörsjlö E, et al. J Biol Chem. 2013;288(47):33997–4008.
- Blom DJ, O'Dea L, et al. J Clin Lipidol 2018;12(5):1234–43.
- Gaudet D, Brisson D, et al. N Engl J Med. 2014;371(23):2200–6.
- Goldberg RB, Chait A, et al. Front Endocrinol (Lausanne). 2020;11:593931.
- Paragh G, Németh Á, et al. Lipids Health Dis. 2022;21:21.
- Spagnuolo CM, Hegele RA, et al. Expert Rev Endocrinol Metab. 2024;19(4):299–306.
- Gouni-Berthold I. J Endocr Soc. 2020;4(2):bvz037.
- Davidson M, Stevenson M, et al. J Clin Lipidol. 2018;12(4):898–907.2.
- Virani SS, Morris PB, et al. J Am Coll Cardiol. 2021;78(9):960–93.
- Pallazola VA, Sajja A, et al. Eur J Prev Cardiol. 2020;27(19):2276–80.
- Veliadkis N, Stachteas P, et al. Pharmaceuticals (Basel). 2024;17(5):568.
- Gaudet D, Stevenson M, et al. Lipids Health Dis. 2020;19(1):120.
- Brinton EA, Eckel RH, et al. Atherosclerosis. 2025;403:119114.
- Stroes E, Moulin P, et al. Atheroscler Suppl. 2017;23:1–7.
- Ginsberg HN, Packard CJ, et al. Eur Heart J. 2021;42(47):4791–806.
- Falko JM. Endocr Pract. 2018;24(8):756–63.